Dr Inderpal Singh, Consultant Geriatrician, Aneurin Bevan University Health Board, National Clinical Lead, Bone Health, Wales
Fracture Liasion Service (FLS)
Strategic Case for Adoption:
Between 2011 and 2021, Wales saw a significant demographic shift, with a 17.7% increase in the population aged 65 and over. This ageing population is particularly vulnerable to osteoporotic fractures, a condition that affects 1 in 2 women and 1 in 5 men over the age of 50, primarily impacting the hip, spine, arm, and forearm.
Notably, the incidence of fractures has risen, with a fragility fracture occurring every minute, compared to every two minutes in 2013. Across the UK, over 300,000 fragility fractures occur annually, costing an estimated £2 billion. In Wales alone, 20,000 fractures are expected each year as a consequence of osteoporosis, which now affects 3.8 million people across the UK.
The scale of the problem: only 9.3% of individuals in Wales who experienced a fragility fracture were identified in 2020 and only 64% received specialist care within 90 days, despite these fractures being a key indicator of increased risk for future breaks. Additionally, only 5.3% of those identified were commenced on treatment and only 20% of these patients were followed up at 52 weeks. This means that only 3.3% (n=222) of patients identified in 2020 received the recommended treatment to guidance (taken from the FLS database).
A 2004 study on fracture risk following an initial osteoporotic fracture found that 34% of individuals aged 60 to 80 years experienced a subsequent hip, clinical vertebral, forearm, or shoulder fracture within the first year. Over a five-year follow-up period, this risk gradually declined to 9% by the fifth year (Johnell O et. Al. 2004).
A study conducted in 2019 among women aged 65 and older found that, in the absence of appropriate secondary prevention, the risk of refracture remained alarmingly high—reaching 10% at one year, 18% at two years, and 31% at five years (Balasubramanian A et. Al. 2019).
A more recent systematic review and meta-analysis in 2024 assessing the effectiveness of FLS in adults aged 50 and older found moderate-certainty evidence that FLS significantly reduces the risk of secondary fragility fractures at follow-up periods of two years or more. Hence stronger partnership and collaboration with Primary Care for an extended follow-up is particularly beneficial due to the time required for bone remodelling as a result of osteoporosis medications (Danazumi MS et. al. 2024).
Proactive care can prevent many fragility fractures, yet the consequences of fractures remain severe and often unmeasurable. Hip fractures are associated with a 20% mortality rate within one year, 50% are unable to walk unaided and 15% require discharge to nursing homes. Additionally, 66% of patients with vertebral fractures develop chronic back pain with 20% risk of dying within five years. Beyond the physical impacts, these fractures also contribute to a loss of confidence, fear of falling, loneliness, and depression.
The economic burden of all fragility fractures in Wales is substantial, amounting to £133,062,444 annually. This figure underscores the importance of addressing osteoporosis and fragility fractures on a national level through preventative strategies and timely interventions.
New Service Approach:
The Fracture Liaison Service (FLS) aims to deliver ROS 80% identification/50% treatment/80% monitoring model for preventable osteoporotic re-fractures. The approach is scalable to all health boards and meets national guidelines.
Methodology:
- Digital identification: An administrator completes an initial triage of a live digital record, identifying patients over 65 years who have sustained a fragility fracture, (the FLS ultimate aim is to identify patients over 50 years). A bone health nurse practitioner/ advanced clinical practitioner (ACP) completes the next review to identify patients who would benefit from a specialist bone health review, whereby patients are referred to a consultant geriatrician.
- Treatment: Suitable patients are contacted for a bone health assessment which includes falls risk and community care. Bone therapy is recommended for suitable patients.
- Adherence to Treatment: Patients will be monitored in their understanding of the risk of osteoporosis, lifestyle modification requirements and their adherence to bone therapy at 16 and 52 weeks.
The service is integrated with radiology, rheumatology, emergency and trauma and patients are seen by the FLS team within days rather than the traditional referral model of weeks to months before their first clinical review.
Clinic & Systems Impact:
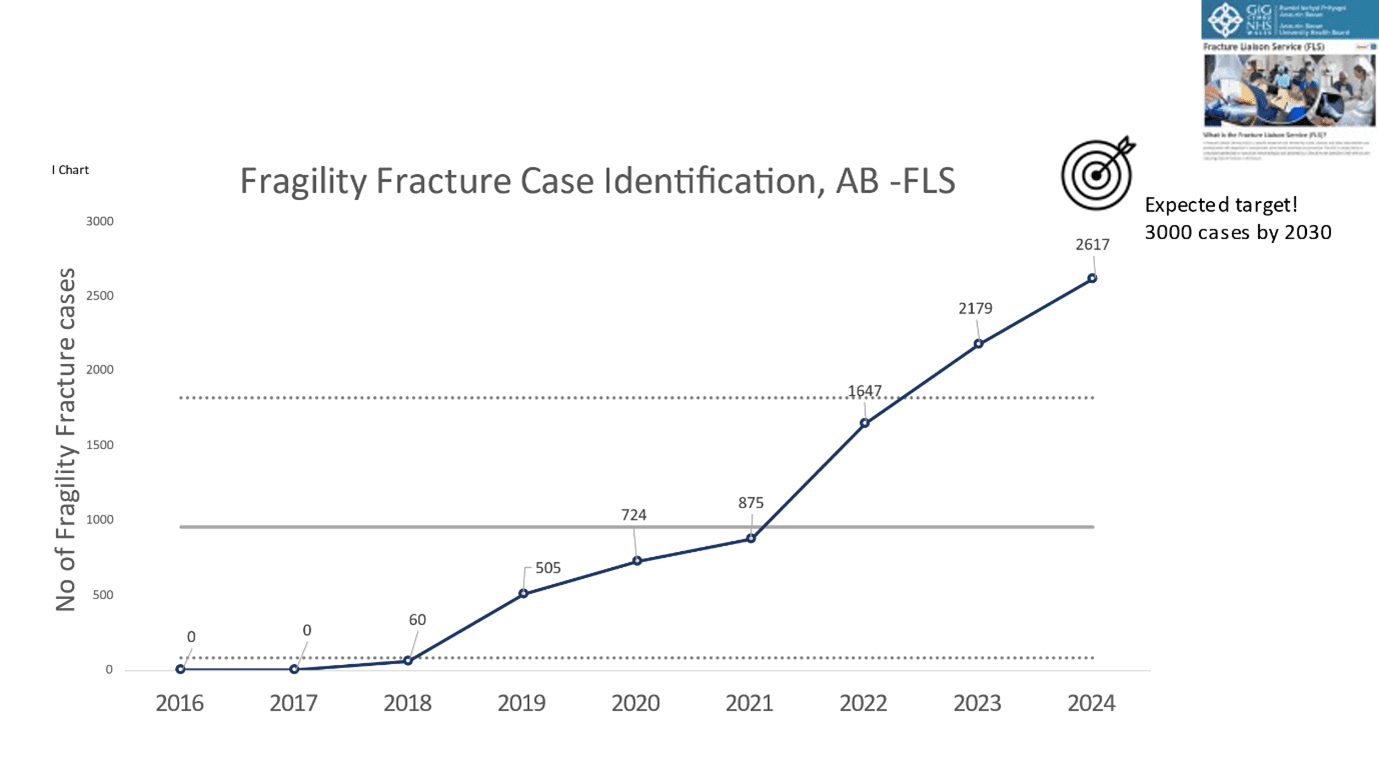
- As a result of the service transformation in Aneurin Bevan UHB, fracture case identification improved from 25% (2021) to 44% (2022). Identification of fracture cases increased further to 53% in 2023, reaching 70% in 2024 (National benchmark=36%).
- 64% patients were treated to guidance (national benchmark=55%). Treatment and monitoring achievement in AB-FLS is now higher than the national average.
- These advancements have ensured that more patients receive timely, high-quality osteoporosis care, preventing missed treatment opportunities.
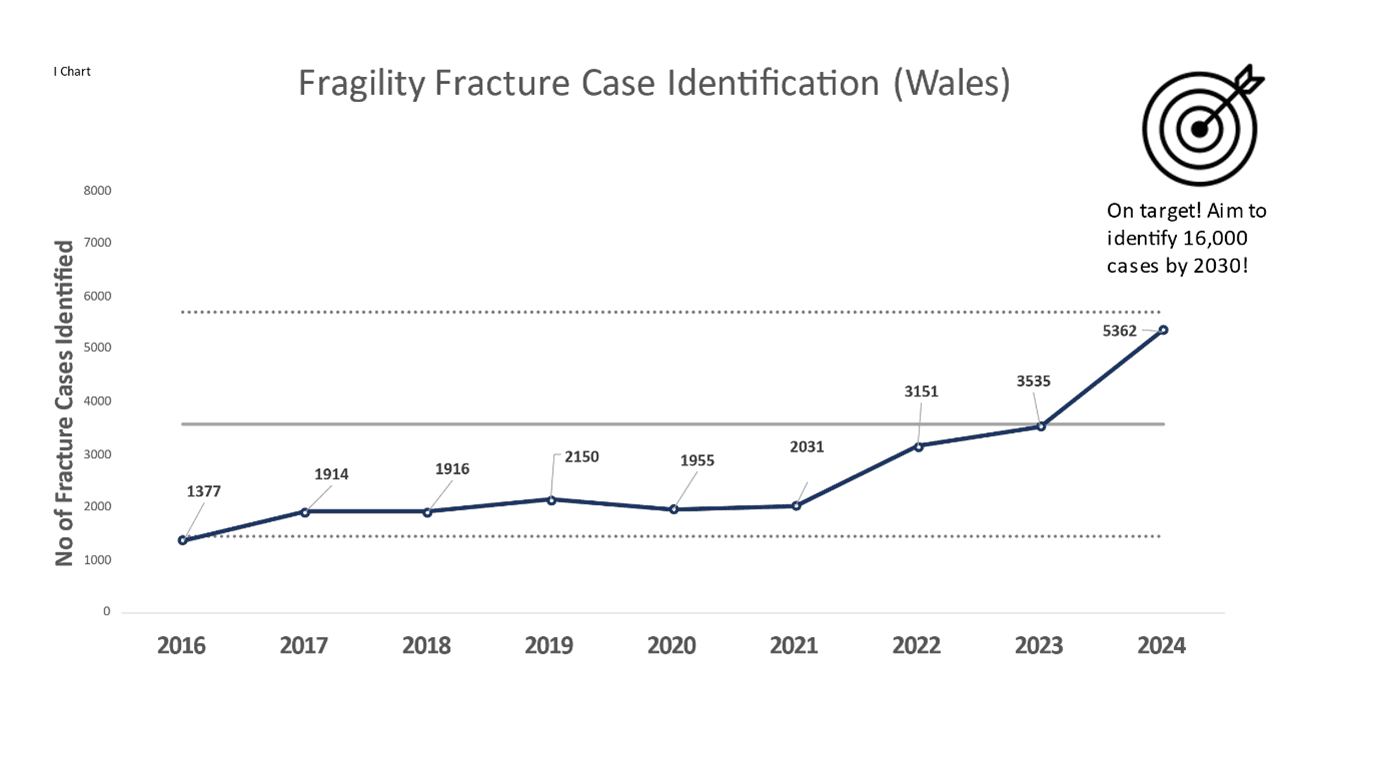
- FLS is spreading across all parts of Wales and there is an observed increase in case identification of 46.5%, from 16.8% (3,537 cases) in 2023 to 25% (5,200 cases) in 2024.
Economic Impact – Local to National Transformation:
The FLS has been communicated as a ministerial priority and has received £1,000,000 funding for national roll out based on its evidence in providing high-value, high-quality patient care. Health boards are expected to consider formal FLS business case to ensure the sustainability of the prudent value based service.
To date, the FLS has recruited an additional 13 ACP/ bone health nurses and 11 administrators/ FLS coordinators.
The FLS has demonstrated a best return of value for services, with expected annual cost benefits of £11,047,324 across Wales.
Key Requirements:
The ROS recommends 1 WTE nurse/ ACP with 0.5 administrator to serve a population between 40,000-46,000.
Key team members:
- FLS administrators/ co-ordinators
- Clinical specialist nurses/ ACPs
- Booking clerks and directorate support officers
- Radiographers
- Consultants (bone health specialists and radiologists)
Benefits:
- Reduced risk and rate of fragility fractures for Wales
- Reduced rate of post fracture mortality and complications that would usually occur in the frailer population
- Reduced demand for primary and secondary services
- Improved patient self management, outcomes and quality of life in older years
- National equitable value-based service with significant return on investment through resource release
- Meeting national standards of care
- Political support for adoption, scale and spread (quality statement and national mandate)
Resources for Health Boards
Relevant Policy/ Strategic Alignment
Quality statement for osteoporosis and bone health [HTML] | GOV.WALES
Our Programme for transforming and modernising planned care and reducing waiting lists in Wales (2022).
Goals:
- Effective referral (most clinical needs seen in the right setting)
- Advice and guidance (to aid informed decision making by secondary and primary care)
- Treat accordingly (right place, right time)
- Follow up accordingly
- Measure what’s important
Priorities:
- Transformation of outpatients
- Prioritisation of diagnostic services
- A focus on early diagnosis and treatment of suspected cancer
- Implementation of a fair and equitable approach to patient prioritisation
- Eliminating long waiters at all stages of the pathway
- Building planned care capacity
- Appropriate information and support
Welsh Innovation Strategy (2023)
Priorities:
- Diagnostics
- Reducing waiting lists
- Reduced time in hospital
- Supporting a talented workforce
Promote, prevent and prepare for planned care (2023):
Supports:
- Advice and guidance to patients and individualised care along the pathway
- Efficiency of care
- Population health and prevention
NHS Wales Technical Planning Guidance 2025 – 2028
Supports the ministerial priorities – ‘timely access to care’ and ‘population health and prevention’
Nationally Available Information:
Royal Osteoporosis Society – Better Bone Health for Everybody
Service Presentation Material:
Dr I Singh Welsh FLS Presentation
Service Implementation Material:
Case for change (full business case available on request)
ROS National Clinical Standards
Fracture Liaison Service Database (FLS-DB) | RCP
FLS-DB resources for services | RCP
FLS-DB resources for service improvement | RCP
Written Statement: Quality Statement for Osteoporosis and Bone Health (6 December 2024) | GOV.WALES
Media:
Videos
Patient’s Voice – Melinda’s Story – YouTube
Articles:
Elderly falls: Wales action to cut costly home fractures – BBC News
£1m investment in FLS for Wales!
Quality care for everybody – Fracture Liaison Service: an all-Wales approach | RCP
A vision for better bone health in Wales | RCP
Royal Osteoporosis Society | Working together to close the care gap
Awards:
First Minister announces finalists of St David Awards 2025 | GOV.WALES
Shortlisted for NHS Sustainability Awards 2025
MediWales Health and Care Judges Award 2024