Mr Alan Treharne, Consultant Gynaecologist, Hywel Dda University Health Board
Enhanced Community Gynaecology Service – Using point of care diagnostics to deliver prudent local healthcare
Strategic Case for Adoption:
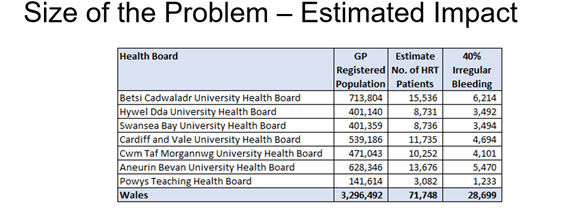
Establishing enhanced community gynaecology services (ECGS) is central to Wales’s strategic national objectives of delivering care closer to home. This project evolved to develop a specific solution to the problem of irregular bleeding in users of hormone replacement therapy (HRT). This issue was putting pressure on cancer services to which an innovative service solution was provided.
Current evidence indicates that 40% of patients commenced on a continuous combined HRT may experience irregular bleeding and where this does not settle, further investigation is required. Hywel Dda has received over 600 referrals in the past 12 months due to issues related to menopause, while the problem of irregular bleeding was directed to the general gynaecology service via the “urgent suspected cancer” pathway. This referral pathway is not sustainable as current evidence indicates that patients on HRT are at a reduced risk of endometrial cancer (the treatment is protective). This clinically inappropriate use of suspected cancer pathways delays diagnosis for other patients.
Based on evidence to date it is expected that 8% of the Welsh population on HRT will be referred to secondary care with irregular bleeding. This would equate to approximately 2295 new cases a year that is being driven into cancer pathways. Eight national ECGS clinics running one clinic a week would meet this patient need.
Methodology:
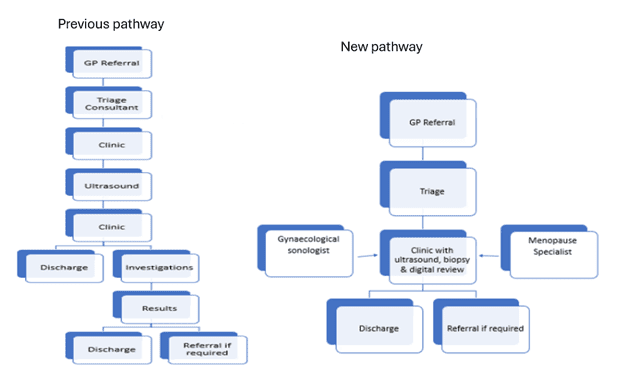
ECGS offers a comprehensive range of outpatient diagnostic and treatment services through a streamlined, consultant-led model. A key focus of the service is the management of irregular bleeding associated with HRT.
Services Provided:
- HRT Irregular Bleeding Clinic: This clinic, equipped with ultrasound, minor procedure, and biopsy facilities, specifically addresses irregular bleeding linked to HRT. It has significantly alleviated pressure on urgent suspected cancer (USC) services and has been highlighted in planned care meetings.
- Mixed Gynaecology Clinic: Designed to address conditions such as endometriosis, polycystic ovary syndrome (PCOS), pelvic pain, and heavy menstrual bleeding, this clinic combines ultrasound diagnostics with consultant-led care. Patients benefit from immediate access to a gynaecologist who can formulate a management and treatment plan in a single visit, incorporating biopsy capabilities where necessary.
- One-Stop Hysteroscopy/Ultrasound Clinic: This clinic facilitates the rapid triage and diagnosis of high-risk patients on cancer pathways, providing a one-stop solution for hysteroscopy and ultrasound needs.
- Additional Services: While not detailed here, other integrated clinical services are also available within the ECGS framework.
The development of this clinic model involved the creation of new referral pathways and guidelines, specifically for bleeding related to HRT. This work has been undertaken collaboratively at an All-Wales level, utilising health pathways to ensure consistent, high-quality care.
The clinical team comprises a Consultant Gynaecologist with expertise in menopause care, supported by a Band 5 Nurse. The clinic operates a paper-free system, with all notes and outcomes recorded on the Welsh Clinical Portal (WCP) for efficient data management, adherence to information governance standards, and streamlined communication with primary care.
Investigation results are received electronically by the consultant, allowing real-time action. This has significantly reduced the time taken to communicate results to both patients and GPs, improving overall service efficiency.
Clinic & Systems Impact:
The work strongly aligns with Wales’s priority of moving care into the community and improving outcomes in women’s health.
- Gynae conditions assessed with a treatment plan provided in one visit, in the community setting
- Improved patient experience and clinician satisfaction
- Significant resource release for radiology capacity
- Clear value savings
- Reduction of cancer referral wait times and increased USC capacity
Economic Impact:
A solution-based approach to a common problem with a significant healthcare and financial impact on both the service and service users. The innovative work has proven financial viability and cost savings and is ready for upscaling.
Hywel Dda Value-Based Health calculated the following economic benefits:
- Resource released per patient: £268
- Resource release over the project period: £73,968 (based on one clinic a week for 46 weeks with a single consultant)
- Resource release impact if scaled nationally – £4,438,080
Key Requirements:
- Gynae Consultant 1FTE per health board, 1 clinic day per week
- Nursing Support
- Administration
- Clinic space 1 day per week
- Ultrasound imaging equipment
Note: Ultrasound equipment has been secured centrally for each health board to implement the service
Benefits:
- Reduced need for in-hospital treatment and inpatient operating, providing care closer to home
- Removed burden from an inappropriately used USC pathway to treat patients with a benign pathology
- Reduced burden of diagnostic radiology – clinician delivered ultrasound is easing delivery pressures in the radiology department where there is a well-established shortage of sonographers in Wales and the UK
- Reduced patient backlog and improved patient flow
- Paper-free working produces a significant impact on notes transport and hence greener healthcare
- Reduced socio-economic burden of patient travel to multiple appointments
- Improved patient experience /outcomes
Opportunities:
The enhanced community gynaecology team plan to work with consultants in the departments of sexual and reproductive health and gynaecology to scale the service as well develop strong links with primary care. The ECGT will also support education and training in Wales with the deanery and will support recruitment and retention.
Resources for Health Boards
Call to Action:
Call to Action Welsh Government
Relevant Policy/ Strategic Alignment
Our Programme for transforming and modernising planned care and reducing waiting lists in Wales (2022).
Goals:
- Effective referral
- Treat accordingly
Priorities:
- Transformation of outpatients
- Prioritisation of diagnostic services
- A focus on early diagnosis and treatment of suspected cancer
- Implementation of a fair and equitable approach to patient prioritisation
- Eliminating long waiters at all stages of the pathway
- Building planned care capacity
- Appropriate information and support
Welsh Innovation Strategy (2023)
Priorities:
- Diagnostics
- Reducing waiting lists
- Reduced time in hospital
- Care closer to home
- Supporting a talented workforce
Promote, Prevent and Prepare for Planned Care (2023):
Supports:
- Advice and guidance to patients and individualised care along the pathway
- Improved efficiency of care
- Increased service capacity
- Improved health outcomes
- Collection of data
NHS Wales Technical Planning Guidance 2025 – 2028
Supports the ministerial priorities – Timely Access to Care and Women’s Health
Service Presentation Material:
Enhanced Community Gynae Clinics Presentation
Enhanced Community Gynae Clinics Bevan Exemplar Poster Presentation
Useful Publications:
Overview | Menopause: identification and management | Guidance | NICE
Management of unscheduled bleeding on hormone replacement therapy (HRT) – British Menopause Society
Service Implementation Material:
Available upon request:
Service implementation plan and materia
Welsh Government Health and Social Care on X: “🙋♀️ The first women’s health hub has opened in Aberystwyth – bringing menopause, menstrual health and contraception support closer to home. More hubs will follow, with one in every health board by March. A big step forward for #WomensHealth. 👇 https://t.co/FdiCFUdRtR https://t.co/WVAYrzKmxQ” / X
Policy:
Women’s and Girl’s Health Quality Statement
Press release ‘Women’s Health Plan launched to close the gender health gap’
Women’s health hubs offer a scalable, equitable future for gynaecological care
Testimonials:
”This is an exemplar project demonstrating proof of principle that services can be delivered more effectively in the community, with better health outcomes and at a lower cost. It’s a testament to outstanding leadership and a relentless passion for delivering the highest quality of patient care”.
Neil Wooding, Chair, Hywel Dda University Health Board
Awards:
Shortlisted for NHS Sustainability Awards 2025 ‘Service of the Year’
Winner of 2025 Hywel Applause Award for Innovation and Excellence
Conference:
Speaker at Women’s Health Ultrasound Imaging Event 22-23 October, 2025, hosted by the National Imaging Academy.